About Dr. Jenson Mak
Dr. Jenson Mak PhD(USyd)MBBS FRACP FACP FAFRM(RACP) BMedSci JP works as a Consultant Physician, Geriatrician, and Rehabilitation Physician in and near the Sydney metropolitan and Central Coast regions.
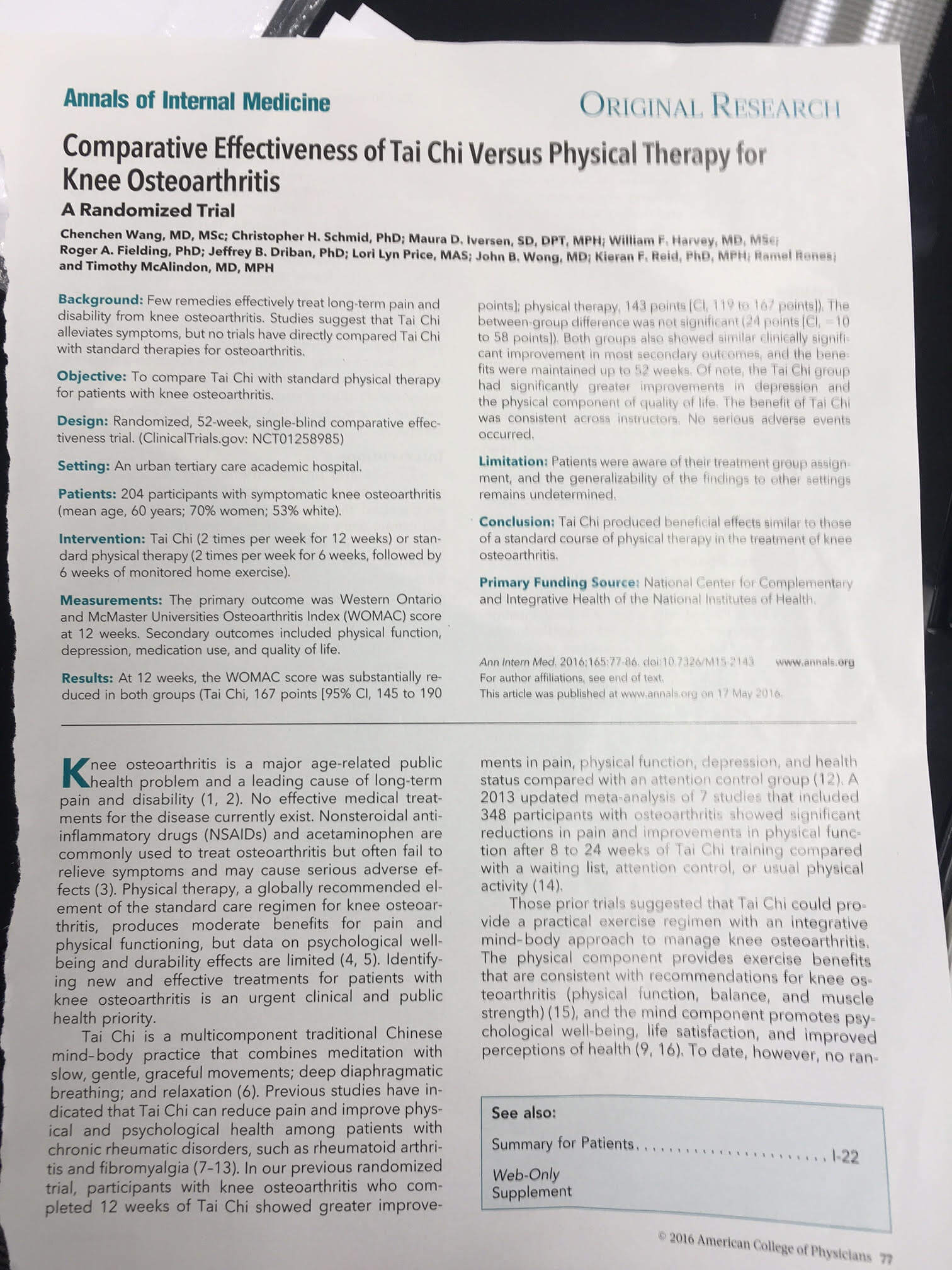
He has more than two decades of experience in the medical field. Jenson Mak’s published work has covered vitamin D, osteoarthritis, osteoporosis, stroke, hip fracture, hip and knee disorders, and holistic medicine. His expertise also details best practice guidelines for general practitioners, specialists, and other healthcare providers who serve patients battling conditions like osteoarthritis and hip fracture.
 Jenson Mak has been elected to Fellowship and travelled to Washington D.C. for Convocation into the American College of Physicians in May 2016.
Jenson Mak has been elected to Fellowship and travelled to Washington D.C. for Convocation into the American College of Physicians in May 2016.
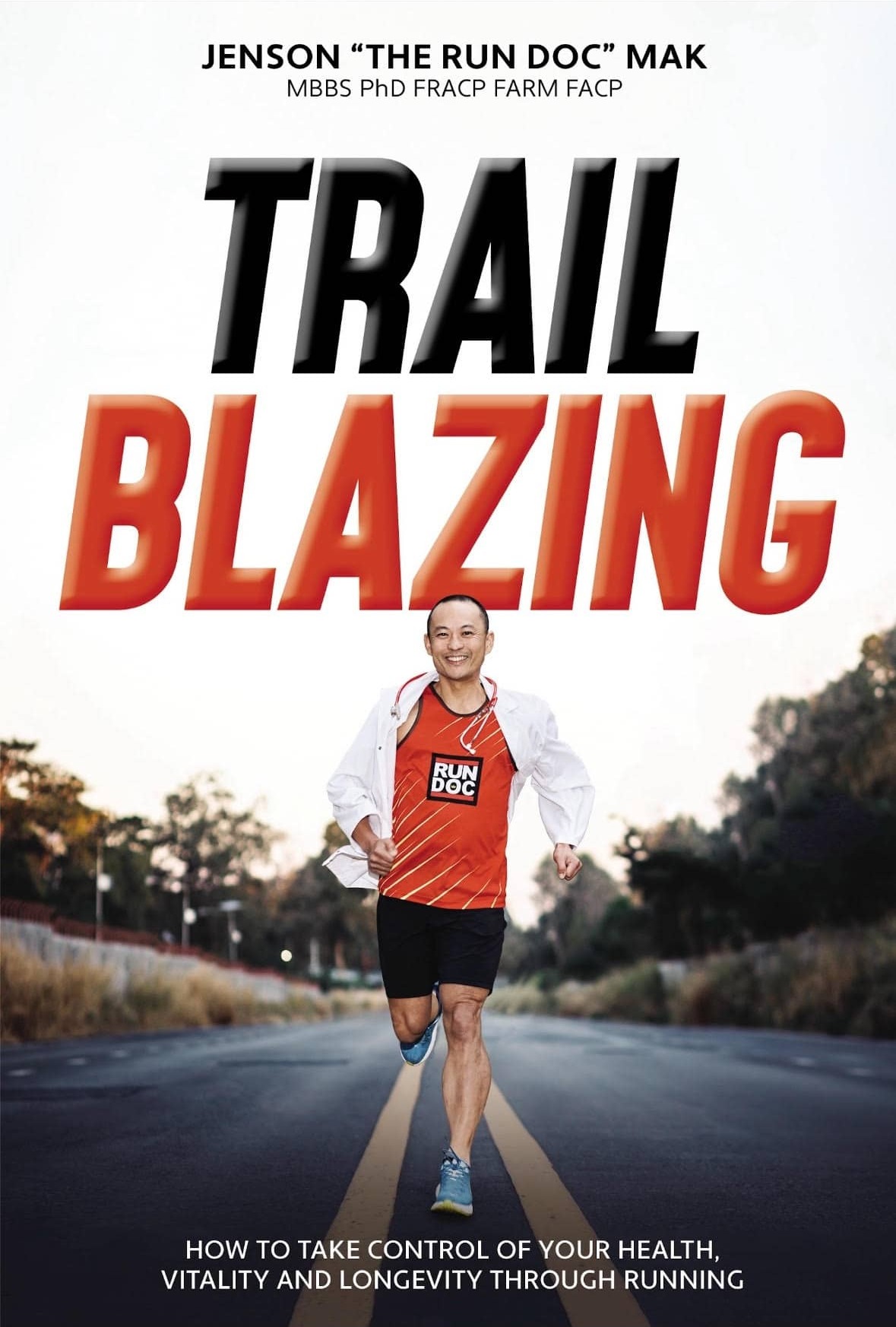
Most recently, Jenson Mak has unveiled his compelling journey in the form of the newly released book, “Trailblazing.” Once known as ‘The Fat Doc,’ grappling with excess weight and a penchant for chocolate, Mak’s narrative unfolds as a remarkable testament to resilience and self-discovery. Motivated by the desire to witness his third child’s growth and break free from a family legacy of premature heart attacks, he transformed his sedentary life into a dynamic adventure fueled by a newfound passion for running. This captivating story invites readers to join Mak on the path of triumph over adversity, celebrating the profound transformation artfully captured in the pages of his latest release.
Read more about this book and purchase a copy for yourself at TheRunDoc.com.au!
A strong believer in the power of preventative medicine, Dr. Jenson Mak emphasizes the complementary relationship between traditional and holistic approaches to healthcare and wellbeing. Traditional medical science assumes only two states of being – “sick” or “healthy.” However, it is important to recognize that even when you are not actively in the throes of illness, you may still be far from well. Holistic medicine extends beyond this overly simple binary and identifies a gray area in between dubbed “un-health.” Areas of un-health can rapidly deteriorate into unpleasant conditions.
In contrast, vitality encompasses a well-rounded approach to nurturing both a strong body and a sharp mind. Dr. Jenson Mak’s professional and academic expertise encompasses a wide enough spectrum to empower him to guide patients towards achieving that goal. Whereas many healthcare professionals overemphasize a symptom-centric approach, Dr. Mak considers the big picture. His passion is finding the root of the problem, and resolving it in a way that can create lasting change. Through fostering real relationships with his patients and their caregivers, he uniquely understands the value of thinking outside the box. Complementary practices like acupuncture, musical therapy, massage therapy, or psychotherapy can better equip many people to achieve a more vital and healthy lifestyle.
On the other hand, it is important to appreciate the value that traditional Western medicine and research does offer. Alternative medical practitioners have the unsavory tendency to overpromise and a relative deficiency in properly conducted clinical trials. However, when you marry the best that both worlds offer, patients win.
Providing helpful, useful information is one of the best aspects of working as a healthcare professional. Dr. Jenson Mak most loves proving to clients that just because a conventional doctor might suggest recovery or improvement is impossible, that does not make it true. Life happens outside of books. Working in a capacity that enables him to rehabilitate and care for some of Australia’s most valuable and inspiring community members is a true privilege. As one of the only medical care providers with his unique cluster of skills, Jenson Mak is proud to be in a position to make a big difference in healthy ageing.
Inpatient Consultation Services
Outpatient Consultation Services
Community Eductation
Medicolegal Reporting
Consultation Locations
CHATSWOOD
Level 1/7 Help St, Chatswood, NSW 2067
Contact: Tel: (02) 9415 2899 Fax: (02) 9415 2199
SYDNEY CITY
Sydney NSW
Tel: +61 2 9282 9725
Fax: +61 2 9252 9721
Enquiries
jenson.mak.chatswood@gmail.com
jenson.mak.centralcoast@gmail.com
jenson.mak.campsie@gmail.com
Preventative medicine ('How to live longer and happier')
Healthy ageing
Hip/Pelvic fracture rehabilitation
Neurological rehabilitation (e.g. stroke, post neurosurgery)
Conservative management of Spinal Pain (back & neck)
Musculoskeletal rehabilitation for conditions not requiring surgery, such as sprains, strains, minor/moderate injury.
Cardiac and Respiratory Rehabilitation
Rehabilitation of the Older Person, after physical deterioration (deconditioning) due to any medical or surgical illness
Injury rehabilitation, such as work injuries, or other accidents
Orthopaedic rehabilitation (e.g. after joint replacement surgery for knees, hips, shoulders, and fractures, joint fusion surgery, and common spinal surgeries
Psychogeriatrics including dementia, depression and anxiety disorders
Osteoporosis and other fractures
Chronic Pain Syndromes
Amputees
In The News
- ACP Convocation Ceremony
- Comparative Effectiveness of Tai Chi
- ACMA's Gift
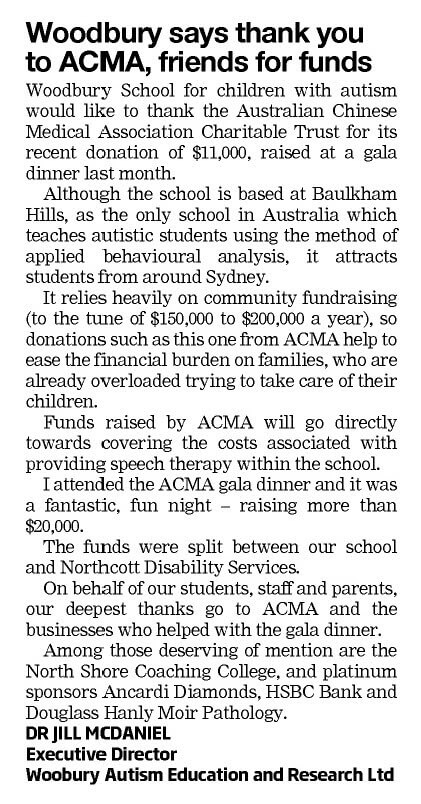
- Thank You to ACMA
- Woodbury School
- 20th Anniversary of ACMA
The American College of Physicians Convocation Ceremony took place in May of 2016. Dr. Jenson Mak is a PhD(USyd) MBBS FRACP FACP FAFRM(RACP) BMedSci JP. He has been elected to Fellowship and was honored to travel to Washington D.C. for Convocation into the American College of Physicians.

The Convocation of the American College of Physicians is an annual ceremony whereby the College recognizes and applauds its new Fellows and the recipients of various honors, including Masterships and Chapter and National Awards. It is a ceremony of tradition, transition, renewal, and celebration.
On Tuesday, 20 November the Australian Chinese Medical Association (ACMA) made an $11,000 donation to Northcott, to enable the not-for-profit organisation to continue to support people with disabilities and their families across NSW and the ACT.
This generous contribution came following the ACMA Charitable Trust’s 20th anniversary Gala Dinner, which was held on Saturday 3 November at the Ted Hopkins Room of the Crystal Palace at Luna Park, Sydney. Read more below.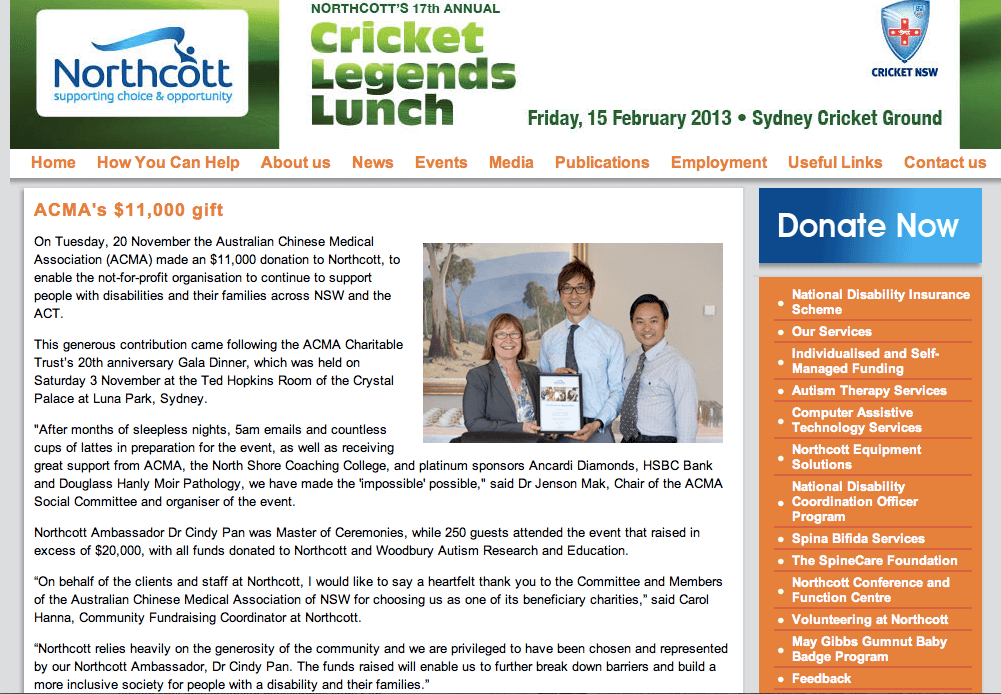
Grateful: Woodbury School at Baulkham Hills received $11,000 from the Australian Chinese Medical Association Charitable Trust recently. The association held a gala dinner on November 3 to raise money for Woodbury and Northcott Disability Services in North Parramatta. More than 250 ACMA members, their families and friends dug deep to raise more than $20,000 in total. Woodbury executive director Dr Jill McDaniel said the school relies heavily on fundraising in the community ‘‘We are thrilled the trust chose us as a recipient of the ball fundraiser,” Dr McDaniel said.
Two-hundred-and-fifty members, partners and friends of the Australian Chinese Medical Association (ACMA) packed the Crystal Palace at Luna park on Saturday 3 November. They were celebrating the 20th anniversary of the ACMA Charitable Trust with guests of honour Mr John Alexander MP, Federal Member for Bennelong (representing the Coalition Deputy Leader, Hon Julie Bishop MP), and the Hon Victor Dominello MP, NSW Minister for Citizenship and Communities, and Minister for Aboriginal Affairs. ACMA also received best wishes for this event from the Hon Julia Gillard MP, Prime Minister of Australia, Her Excellency Prof Marie Bashir, Governor of New South wales, and the Hon Barry O’Farrell MP, Premier of New South Wales.
The party goers were thoroughly entertained by the incredible band ‘Beatles Magic’. Dr Cindy Pan (Ambassador for Northcott Disability Services and Chair for Charitable Trust Subcommittee of the ACMA) was Master of Ceremonies, and through her efforts and those of Auctioneer extraordinaire Mr Tony Hanlon, the event raised in excess of $20,000 for two organisations providing vital support and services for children with disabilities, the Northcott Disability Services and Woodbury Autism Research and Education.
This auspicious event was organised by Dr Jenson Mak, Chair of the ACMA Social Committee.
“After months of sleepless nights, 5am emails and countless cups of lattes in preparation for the event, as well as receiving great support from ACMA , the North Shore Coaching College, and platinum sponsors Ancardi Diamonds, HSBC Bank and Douglass Hanly Moir Pathology, we have made the ‘impossible’ possible” Dr Mak says.
The Australian Chinese Medical Association is an established professional and social organisation comprising doctors and specialists from New South Wales, its website is www.acma.org.au.

Convenor of 2012 ACMA Gala Dinner (Dr Jenson Mak), with Hon Victor Dominello MP (NSW Minister of Citizenship & Communities), Dr Cindy Pan (MC & Ambassador for Northcott Disability Services) & her 2 children, & Mr John Alexander MP (Federal Member for Benelong)
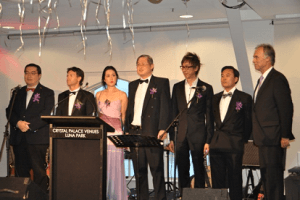
ACMA Gala Dinner Singing the National Anthem: ACMA President Dr Danforn Lim, with Hon Victor Dominello MP (NSW Minister of Citizenship & Communities), Dr Cindy Pan (MC & Ambassador for Northcott Disability Services), Dr Seng Chua, Dr Stephen Hing , Dr Jenson Mak (Convenor of 2012 ACMA Gala Dinner & Chair of Social Commitee), & Mr John Alexander MP (Federal Member for Bennelong)
Dr. Mak's Published Work
High Fitness Levels Linked to Decrease of Cancer Risk
It is no secret that frequent exercise and daily physical activity is good for your health. Exercise can help with weight control, mental health, and is overall good for the soul. Along with all the commonly known health benefits of regular fitness, it has now been...
Dancing Promotes Healthy Ageing in Mind and Body
It is certainly no surprise that exercise is directly linked to the health and wellness of ageing adults. In order to keep both mind and body functioning correctly, you must continue to do activities that promote movement in the brain as well as your joints and...
Early And Regular Exercise Eases Osteoarthritis Knee Pain
The most common type of arthritis, osteoarthritis, affects in excess of 30 million Americans. Harvard Medical School cites these statistics while recommending ways to avoid or alleviate the condition. The institution notes two significant factors that affect patient...